LONDON (Reuters) – UK scientists seeking approval to deliberately infect healthy people with COVID-19 in trials must first convince ethics specialists that, among other things, they have potential “rescue therapies” or antidotes to halt the disease.
The problem is that, for the novel coronavirus, there is still no effective treatment or cure.
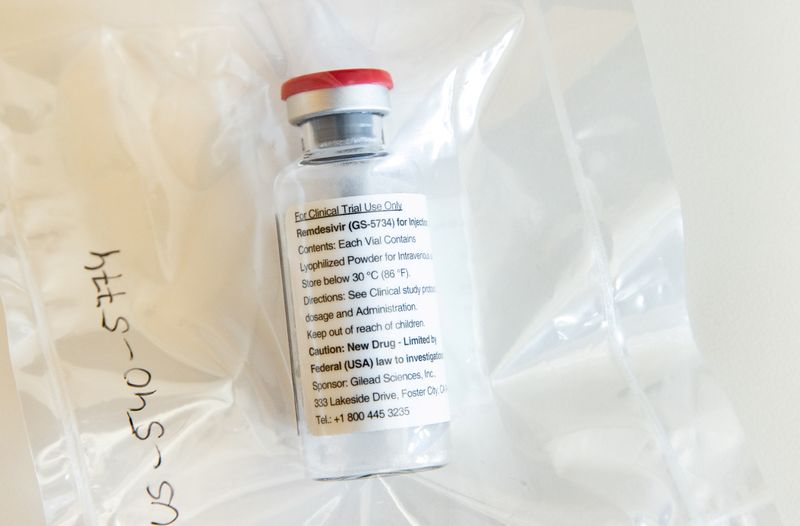
That means, for now, that the best scientists planning the so-called human challenge studies can offer is Gilead’s remdesivir – an antiviral drug that was found in a large trial to have no impact on COVID-19 death rates.
Chris Chiu, a scientist at Imperial College London co-leading the COVID-19 challenge experiments, said the plan was to give remdesivir to infected volunteers based on a “strong belief” it will be effective if given in the very earliest stages of disease.
Some ethics and medicine experts said that posed problems.
“As an effective rescue therapy does not yet exist for SARS-CoV2, there is a serious ethical dilemma … to address here,” said Stephen Griffin, an associate professor in the school of medicine at Britain’s Leeds University.
Other specialists said the lack of antidotes or rescue therapies was only one of several risks the research team would have to minimise, and trial volunteers would have to accept, if the studies are to gain ethical approval.
Plans to reduce those risks include picking the most robust, healthy, young volunteers to be infected, and using the bare minimum amount of the coronavirus to infect them with COVID-19.
Dominic Wilkinson, a professor of medical ethics at Oxford university, said that, while desirable, having an effective treatment at the ready after deliberately infecting volunteers was “not essential for the ethics of such a trial”.
“The ethical necessity of these trials, and of any trial, is that you assess the risks, you minimise the risks, and you communicate the risks,” he told Reuters. “It’s not the case that you have a situation where there are no risks.”
PUBLIC TRUST
Human challenge trials are not new. Scientists have used them for decades to learn more detail about – and develop treatments and vaccines against – several other diseases such as malaria, flu, typhoid and cholera.
“Generally with such trials in the past, they were done when you had a specific treatment,” said Margaret Harris, a spokeswoman for the World Health Organization (WHO), when asked about the planned UK trials using the novel coronavirus.
“You must ensure that everybody involved understands exactly what is at stake … and ensure informed consent is rigorous – that they really do understand all the risks,” she said.
Ohid Yaqub, a science policy expert at Britain’s University of Sussex, pointed to WHO guidelines on the issue, which among other things say human challenge trials “might be considered when the disease an organism causes has an acute onset, can be readily and objectively detected, and existing efficacious treatments … can be administered … to prevent significant morbidity, and eliminate mortality.”
Yaqub warned of a risk to public trust in science and medicine if these criteria are ignored or skimmed over, adding: “There needs to be wider consultation about undertaking such studies.”
He noted that selecting a small number of low-risk participants would mean “fatality, hospitalisation or long-term symptoms are extremely unlikely scenarios”, but added: “Even their remote possibility threatens trust in research and vaccines more than necessary, because public engagement on this issue has been limited.”
(Reporting by Kate Kelland; additional reporting by Stephanie Nebehay in Geneva; editing by Mark Potter)