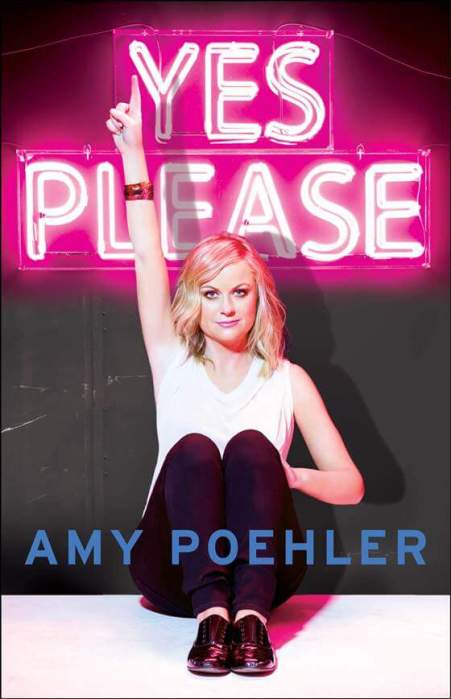
If you have gestational diabetes, you need to carefully monitor it before and after delivery.
If you have gestational diabetes, you need to carefully monitor it before and after delivery.
Credit: Photodisc
Melanie Jay didn’t consider herself at risk of developing gestational diabetes, a diagnosis during pregnancy that means excess blood glucose (sugar) is passing from the mother to her baby via the placenta. A general internist and an assistant professor at New York University School of Medicine and Population Health specializing in obesity-related health services, Jay didn’t have a strong family history of the condition, wasn’t overweight, exercised regularly and maintained a healthy diet. Pregnant with twins, however, she developed gestational diabetes and had it during her next pregnancy as well.
“The influx of placental hormones during pregnancy help your baby develop, but they can also block normal insulin function in the mother, making your body more resistant to insulin,” Jay says. Without enough insulin, your body can’t convert glucose into energy, so it collects in the bloodstream. High glucose levels in the blood can lead to serious pregnancy complications, such as preeclampsia (a high blood pressure condition that if left untreated can be fatal), preterm delivery, overweight babies and an increased risk of cesarean delivery.
The American Diabetes Association estimates that gestational diabetes affects 18 percent of all pregnancies. Some women are genetically predisposed to develop diabetes, particularly if they are overweight, says Dr. Joel Zonszein, director of the Clinical Diabetes Center at Montefiore Medical Center, the University Hospital for Albert Einstein College of Medicine.
Because moms-to-be with gestational diabetes are passing along high levels of glucose via the bloodstream, their babies overproduce insulin; this means they’re getting more energy than needed, which is then stored as fat. Macrosomia, or “large” babies, can injure their shoulders during delivery, are at higher risk of developing respiratory problems and have a greater risk of becoming obese or diabetic later in life.
Women are often good about carefully controlling their diabetes with glucose monitoring, diet and exercise during pregnancy, but it can be more difficult after delivery, when the baby’s health is no longer a factor and they’re overwhelmed with the responsibilities of being a new mom. One study showed that many women don’t get screened to see if they have diabetes after they give birth.
“Many women will have perfectly normal blood glucose levels after pregnancy,” Zonszein says. “But it doesn’t go away forever. Within five years, 50 percent of women who had gestational diabetes will develop Type 2 diabetes.”
Because people are being diagnosed with Type 2 diabetes at younger ages — a fairly recent phenomenon — more women will face additional health risks during pregnancy, Zonszein says. The baby might develop heart abnormalities, for example, and women with Type 2 diabetes often have high blood pressure, which can adversely affect her heart and kidney function and put her at greater risk for infections.
“The medical problems of these women are much more numerous than those of women without preexisting diabetes,” says Zonszein. “Diabetes medications, such as hormones we use to lower the weight of the patient, haven’t been studied [for use] during pregnancy. Often they’re on medications they shouldn’t be taking while expecting.”
Therefore, it’s important for women with diabetes to see their physicians before trying to get pregnant, he says.
“The key is education, not only how to monitor blood sugar levels but what she can expect before, during and after pregnancy,” Zonszein says. “Women should also involve the entire family in learning to control diabetes, because if she has it, chances are her kids will. Prevention is easier than treatment.”