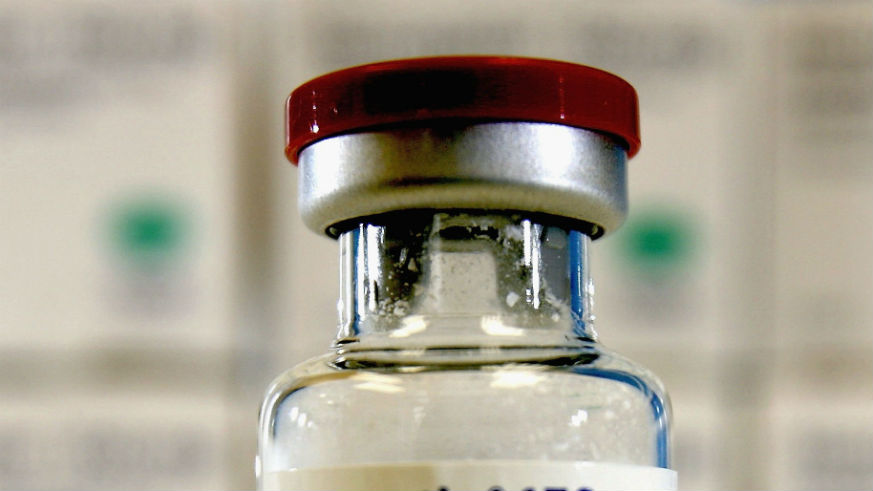
Medicine is supposed to either alleviate symptoms of a disease or help improve quality of life for those who take them, but a new study by researchers in Britain and Latvia show that most of the anticancer drugs on the market don’t do either.
The study — published this month in the British Medical Journal — looked at the 48 cancer medications approved by the European Medicines Agency between 2009 and 2013. The medications, approved as treatments for 68 different situations, were approved based on clinical trials that suggested they might shrink tumors or provide other health benefits for cancer patients.
How many anticancer drugs work?
Instead, the researchers found that only 10 percent of the approved drugs provided measurable improvements in quality of life for cancer patients at the time they were approved — and 57 percent provided no benefits.
Study co-author Huseyin Naci, assistant professor of health policy at the London School of Economics, said that they then looked at how the drugs performed over time.
“We wanted to see once [the drugs] were already on the market did they actually generate some evidence to show that they improved or extended life?” Naci told The Guardian. Those results didn’t improve much: 49 percent of the cancer drugs didn’t help improve survival or quality of life in the three to eight year follow-up period.
“What we find very surprising is that not very many studies are looking at overall survival or quality of life as their [primary] objective,” said Naci. The breast cancer medication Herceptin and Zytiga, used for prostate cancer, were shown to help patients — as were 23 others. However, their ability to increase survival rates were “marginal,” according to the researchers.
Weighing the benefit of anticancer drugs and their cost
Vinay Prasad, an assistant professor of medicine at the Oregon Health and Science University, wrote in a study editorial that the results paint “a sobering picture” of medications that can cost in excess of $100,000 per year of treatment.
“The expense and toxicity of cancer drugs means we have an obligation to expose patients to treatment only when they can reasonably expect an improvement in survival or quality of life,” Prasad wrote, adding that the study “suggests we may be falling far short” and that more rigorous testing based on real-life trials should be used to make sure they’re worth it for the patient.
What should you do if you take anticancer drugs?
Naci said the findings did not mean patients should worry. “I think it is very important that no one is alarmed,” he told The Guardian.
“The study does highlight the importance of using real-world evidence from patients, on top of data from clinical trials, to build our understanding of how drugs work in a real-life setting,” added Emma Greenwood, Cancer Research UK’s director of policy. “We’re already starting to see this happen through the cancer drugs fund in England, where patients can access promising new drugs while more data is collected on their effectiveness.”
This study — though alarming — doesn’t mean cancer patients should stop taking their medicine. Your doctor should make the call on the best course of treatment for your cancer, always.