MassHealth, the state’s program to provide health insurance coverage to low-income residents, made $193 million in improper payments for mental health-care coverage, the state auditor said.
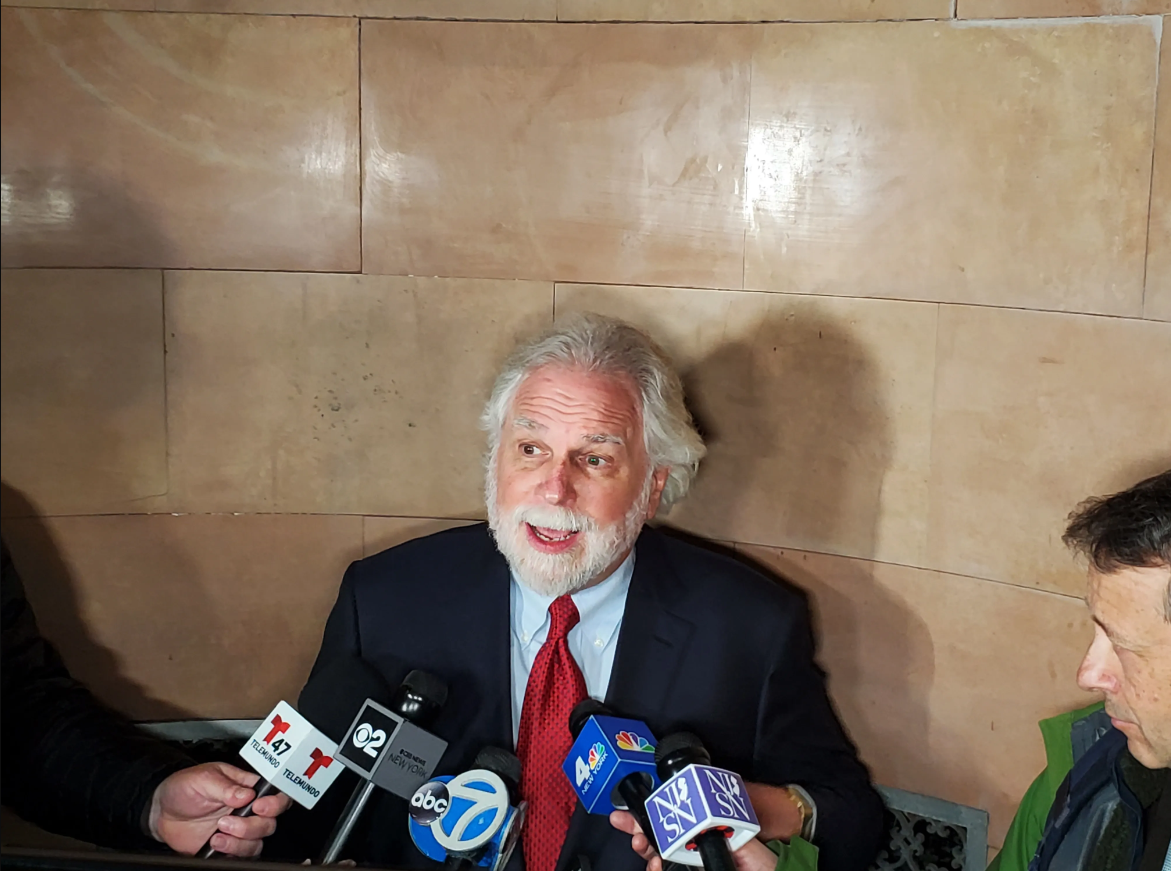
The report, issued Monday by state auditor Suzanne Bump,shows problems with how MassHealth pays for mental health services.
The audit did not accuse the agency of fraud, but instead pointed to duplicate payments for the same services, or confusion about responsibility for payment.
MassHealth has been paying doctors directly for mental health services, although those services should have been paid for by the Massachusetts Behavioral Health Partnership, a company hired by the agency to coordinate mental health care for members. RELATED:Baker eyes penalties for companies that don’t offer healthcare In the 2016 fiscal year, MassHealth paid health-care providers $14.8 billion for services, which covered about 1.9 million people. The program accounts for one-third of the state budget.
“This audit is the latest example of poor claims administration at MassHealth,” Bump said in a statement. “Some of the problems identified stem from MassHealth and its contractors’ different understanding about who is to pay what; other times MassHealth simply acts contrary to its own rules and standards.” MassHealth disagreed with the audit. It said Bump’s office noted in the report that the services in question are not actually part of the rates paid to MBHP. The auditor countered that the office looked at the correct claims. The auditor said changes could end up saving the program up to $27 million a year. “It’s my hope that today’s audit will assist policymakers in their efforts to control costs in this important program,” Bump said. RELATED:Obamacare repeal could leave 500,000 Mass. residents uninsured, protestors say Between July 1, 2010, and June 30, 2015, MassHealth paid MBPH about $2.6 billion as part of a contract that specifies what services and procedures the behavioral health partnership must provide to members. But as MassHealth was making those monthly payments, the audit found that it also paid doctors directly about $93 million for the same services covered in the MBPH contract. That means MassHealth paid for the same services multiple times. The audit also identifies about $100 million in “questionable payments” for items like family therapy sessions, behavioral-health counseling and psychological testing. The auditor’s office said that these services are “clearly behavioral health in nature,” yet were not included in the list of services covered by the contract with MBHP. RELATED: Trump tells lawmakers he expects deal ‘very quickly’ on health care MassHealth regulations require that all behavioral health services be paid for by MBHP, the audit notes.
MassHealth was also found to have paid claims for behavioral health services provided via emergency rooms, instead of referring those claims to MBHP (as required by regulations). This creates a “financial incentive,” the audit says, for MBHP to allow its members to seek behavioral-health care by going to the emergency room. An audit released in 2015 found similar problems with how the MassHealth managed contracts. That audit found that MassHealth unnecessarily paid about $233 million to doctors for services that should have been covered under “managed care organization” contracts. Addressing these contracts and the way MassHealth pays claims would save money, Bump said, which could prevent fees from being raised or benefits from being reduced.
State audit identifies nearly $200M in ‘improper’ payments by MassHealth